The PF Perspectives Library
Here's what patients, caregivers and healthcare providers have to say about living with, and caring for those who live with, pulmonary fibrosis.
Understanding life with PF
Three Lakes Foundation was created by a family tragically affected by pulmonary fibrosis (PF). Driven by their own frustrations with misdiagnoses, lack of information, limited treatment options and challenges with oxygen access, they built an organization focused on driving awareness, accelerating therapies and improving care for PF.
To help solve these problems even faster, Three Lakes Foundation recently partnered with MATTER, a hub for healthcare innovation and entrepreneurship, to help find innovators with new ideas and solutions for PF — and change the experience for patients, their caregivers and healthcare providers.
Below are their stories.
A special acknowledgment to the selected participants who will receive $500 cash prizes and the opportunity to collaborate with PF innovators during the PF Innovation Challenge: Beatrice, Cyril-Patrick, Ed, Maryluz and Max.
Cyril-Patrick, Patient
Challenge: Diagnosis
What type of improvement will make the biggest change in PF? In my experience of a lung transplant, the most pressing issue is time to diagnosis. Currently, primary care physicians (PCP) follow correct procedures, but Pulmonary Fibrosis (PF) goes largely undetected for 4 years. In my case, this causes anxiety, panic attacks, poor quality of life, job loss, hospitalization, and even death. Fortunately, my 40-year career in the semiconductor industry lends itself to use practices of gathering knowledge and embedding it into the software to improve time-to-diagnosis by 4-10X. The underlying problem is that the needed information is unobserved, unrecognized, or insufficient for the PCP to diagnose PF, as this is a rare disease and we practice prescriptive medicine. What is needed is a new innovative approach to collect the right knowledge and embed it into software that is merged with the patient data — ultimately uncovering problems, seen or unseen, that turn out to be major problems. This innovation can revolutionize the medical industry. E.g., Crackles that a pulmonologist can hear but not the PCP, the use of a spirometer to measure breath early for those who cough and have shortness of breath, reading of an X-ray… where one radiologist can recognize IPF and another cannot. Thus, CT scans and X-rays could detect lung issues much earlier. There is a pattern to the X-ray and HCRT that is known to the pulmonologist, but not to the general PCF. The next step is an HRCT scan that a pulmonologist can read at first glance.

Max, Healthcare Provider
Challenge: Quality of Life & Oxygen
Pulmonary fibrosis is a disease that can affect patients of all ages and from all walks of life. As an early career lung-disease specialist, I have seen the effects of this disease first hand, from the frustrating delay of diagnosis which can span months and even years, to the progression of symptoms that can render even the simplest pleasures of life impossible. I enjoy caring for patients in a comprehensive interstitial lung disease clinic and always strive to provide a clear diagnosis and personalized treatment plan for each patient, in order to improve my patient’s quality of life and outcomes. And while the current available treatments certainly help, I also see the limitations of these medications and the challenges my patients face each and every day. These include obtaining expensive medications, ensuring access to a reliable supply of supplemental oxygen, and making sure they can still do things that bring them joy. But the biggest barrier to better care, in my opinion, is our limited knowledge of the causes of pulmonary fibrosis. Because of this, I also spend time in the laboratory performing research to better pinpoint the origins of pulmonary fibrosis. I believe that if we better understood the root causes of pulmonary fibrosis, we would be able to design more effective treatment, transforming the everyday experiences of patients living with pulmonary fibrosis and allow them to live their lives to the fullest. I look forward to working with others in the pulmonary fibrosis community to make this a reality.

Beatrice, Caregiver
Challenge: Oxygen
My husband has had pulmonary fibrosis for many years. It was heartbreaking to have this happen to my husband, who was always my walking partner all around NYC. There are a lot of challenges when going to doctor’s appointments, like getting used to the oxygen equipment. Or getting help from others when problems arise. At a doctor’s appointment, the piece that attaches the oxygen to the portable tank broke off while I was getting my husband a new tank. I was in a hospital and asked the person at the front desk. He told me to go inside and ask a nurse. The nurse had to wait for an available tank. I was frantic because my husband couldn’t breathe without oxygen and I couldn’t get help fast enough. They didn’t have any oxygen available and it would take some time. I had to repair the piece myself by using my teeth somehow, and finally got the piece connected to the oxygen tank. I had to take my husband home right away. I have had many incidents with the tanks — like being unable to tighten the tops and the hissing sounds not stopping. I had to add a washer to the tank. Doctor’s offices and hospitals should have oxygen available right away to people that need it. Also, workers should be more caring and helpful and more oxygen training should be given to caregivers.
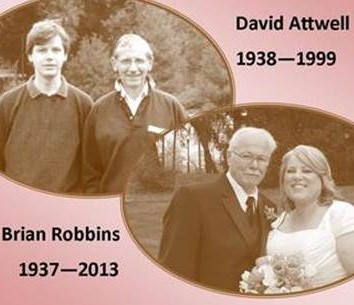
Colleen, Caregiver
Challenge: Diagnosis & Awareness
My husband and I both lost our fathers to IPF. One experience I remember clearly while my father was dying, was the lack of information his doctors had — he lived in a rural area. His primary doctor (whom he saw for other issues) would leave him waiting so long for appointments that his oxygen tank would run out. Primary doctors don’t seem to know what to do or how to deal with IPF patients. It was appalling. We need more doctors who understand this disease and how to deal with PF patients. Information and awareness are key.
Jim, Patient
Challenge: Diagnosis & Coordination of Care
I’m Jim and I was diagnosed with IPF in 2016, (then re-diagnosed with which restrictive lung disease (RLD) in 2018, when a second diagnosis was done at an ILD hospital). I’m not on oxygen and I use a combination of medications to stabilize progression (successfully to date). My biggest challenges have been getting the correct diagnosis and proper treatment, setting up a healthcare team and navigating insurance benefits, all while changing my lifestyle completely. I’ve given up much to realize gains I never realized possible, with the help of my wife who makes it all possible. My lessons so far are: Seek a critical care network hospital for ILDs, and find a local support group or social media group to participate in. The information and knowledge you will gather from others like yourself is priceless. And, take care of your caregiver — they are your strongest supporter.
Joan, Patient
Challenge: Diagnosis & Quality of Life
In December 2014, I went to Grand Rapids to be with family at Christmas and was hospitalized with chronic respiratory failure on Christmas day. After recuperating for a week, I returned to Georgia but really did not feel “over it.” I found another pulmonologist. On June 01, 2015, I was diagnosed with pulmonary fibrosis. Only, my doctor didn’t name it. He just confirmed there was scar tissue present and I would have to wear oxygen forever. He assumed I understood my situation. I was in denial and knew nothing. I stayed in denial for six months. He ordered a biopsy in August of that year. It revealed hypersensitivity pneumonitis, a very non-aggressive form of PF. I was still in denial. I thought I would get over it. When I finally became realistic about the disease, I entered a grief cycle that would last for at least four years. I cried and screamed with anger. I changed my depression medicine at least three times. One of the ways I finally began to cope was to start making art. The disease reduces one’s energy level. When my depression kicked in, I found that art can allow me to express myself. I want to use art with others when they say, “I don’t have the energy to do anything.” I want to help them find a way to use what energy they may have to do something that gives them hope.

Linda, Family Member
Challenge: Diagnosis & Patient Education
I lost my brother, father, grandfather, and two cousins to pulmonary fibrosis. I’m followed for signs of it. My family has talked with families and researchers for nearly 20 years. Patients express fear and confusion about whether their children or siblings are at risk. Estimates are that 13-20% of PF cases are familial. Of 200,000 individuals with PF, 40,000 could have a familial form, each with one or more affected relatives but undiagnosed, or pre-symptomatic but at risk. Early identification is critical — familial patients may progress earlier than sporadic patients; those with short telomeres may have worse transplant outcomes. What’s missing? 1) Researchers’ consensus on surveillance practices to identify and follow relatives at risk, 2) information for families about their risks and options. Proposed: 1) Working groups of researchers, with input from patients and genetic counselors, will generate and publish guidance with A, B, C evidence levels on identification/surveillance: At what age adult relatives of two or more patients should test: e.g., before the 10 year cancer protocol of patient age of onset, to account for genetic anticipation? What testing should include, at what intervals: pulmonary function, HRCTs, ILAs/interstitial lung abnormalities? 2) An e-learning program will disseminate findings, with modules customized by audience: primary care providers, pulmonologists, nurses, patients, genetic counselors. Virtual support groups would allow discussion of concerns. Research has matured to test models and translate findings into action. This approach could calm unwarranted fears, facilitate early detection/treatment, and save lives among an overlooked population.
Malcolm, Patient
Challenge: Fatigue
My name is Mal and I have idiopathic pulmonary fibrosis. I was diagnosed on February 1, 2018. It was a cold day and I started out on my daily walk. After walking a short distance I had trouble breathing and was afraid I would be unable to return home. I made it, went to the doctor, was hospitalized and diagnosed following a CT scan that showed scarring of the lungs. I then became involved with the Pulmonary Fibrosis Foundation, started the Greater Hartford Pulmonary Fibrosis Support Group, became a Pulmonary Fibrosis Ambassador and participated in community events to create an awareness of this disease that “takes your breath away.” For me, the most difficult part of living with Pulmonary Fibrosis is the constant cough and shortness of breath, and fatigue is what bothers me the most. Difficulty sleeping is also a very annoying challenge. I am a very active person and try to hide my health issues. For most people, if you look and act healthy, then you must be healthy. In order to get daily obligations completed it is necessary to start my day early and get everything completed by noon. After that, my ambition level falls off dramatically and I am in need of rest for the remainder of the day. Personally, I feel the key to quality living is to have a positive attitude and fight this disease every single day.
Maria, Patient
Challenge: Awareness
My name is Maria do Rosário. I’m from Lisbon, Portugal and I’m 59 years old. I was diagnosed with pulmonary fibrosis in June 2017 after doing a biopsy. My PF was caused by chronic hypersensitivity pneumonitis. I was a kindergarten teacher and because of the disease, I had to retire. I had never heard about this disease prior to being diagnosed, and nobody from my family ever had PF. It was hard to take it in, especially when I investigated and learned that it was a terminal disease. I had to explore other interests; I write poetry for children and created a page and a support group in Portugal for family members and patients with PF. Today I use oxygen in exertion and deambulation. My pulmonologist wants me to be listed for a transplant… I live one day at a time, enjoying life as best I can and hopeful for advances in medicine.

Martin, Caregiver
Challenge: Diagnosis & Remote Care
My father died from pulmonary fibrosis. Improvements needed are: 1) an early and accurate diagnosis. 2) A test that is easy to administer and primary doctors that know to order the test. 3) Better access to consulting doctors and support teams remotely via video and phone to avoid stress and strain of travel for PF patients.
Sandy, Patient
Challenge: Fatigue, Quality of Life
Hi, my name is Sandy. I was formally diagnosed with IPF and bronchiectasis shortly after a Vats lung biopsy in December of 2015. A few years before, I was having difficulty climbing stairs and becoming so short of breath. It all came to a head while on a vacation in Florida and walking the beach. I stopped in my tracks when I could not catch my breath. I thought I was having a heart attack. So I started my journey to find out what was wrong. After my Vats biopsy I had to get a second opinion as my pulmonologist still didn’t know what was wrong. I am now taking Esbriet and so far my IPF has not progressed — which brings me to my frustration. I see my pulmonologist every six months, I get my chest X-ray, and my spirometry tests. I’m told I’m doing remarkably well. My frustration is that the day to day living is not that great. The constant coughing does not allow me to live the quality of life I would like. The coughing greatly fatigues me and I end up taking one to two hour naps during the day. In addition, the anxiety that comes with this disease is overwhelming. My doctor ordered a percussion vest along with a nebulizer. But the nebulizer makes me violently cough. In addition to all the tests, doctors also need to focus on the IPF cough and the day to day things one deals with when living with IPF.

Sarah, Caregiver
Challenge: Oxygen
Portable oxygen concentrators are heavy and have fixed flow, limited flow capacity, and limited battery life. With advanced IPF, my mother has to use cylinders because her flow needs are not covered by oxygen concentrators. The day revolves around planning outings, filling cylinders, and manually adjusting flow for rest and exercise levels to maintain pulse ox above 90%. Heavy cylinders or oxygen concentrators impact mobility and independence.

Sherry, Healthcare Provider
Challenge: Research
Although National Jewish Health is home to the nation’s largest interstitial lung disease (ILD) clinic, and our physician-scientists are world leaders in classifying and understanding the many types of ILD, those types that involve scarring — also known as pulmonary fibrosis (PF) — are more difficult to treat because less is known about them. Our physicians and researchers are conducting innovative studies to find ways to treat PF more effectively with little to no side effects, and to better understand what causes a person to develop PF. Some causes of PF are known, including auto-immune conditions, specific medications or occupational particulates (such as mining dust), however, a large number of PF cases are idiopathic (i.e., from an unknown origin). Our research is focused on identifying what causes IPF, diagnosing PF early for better outcomes, and finding the best clinical practices for our patients. In order to answer these questions and provide optimal care, extensive research is necessary. Research is expensive and is the number one barrier for providing optimal care for IPF patients. NJH is committed to expanding our research program to meet these needs. Due to our unwavering drive to find answers and our expertise, the National Institutes of Health has designated NJH as a Specialized Center of Research for ILD. Many of our grateful patients have spent years looking for answers to their complex medical conditions and tell us we were the only place that could help. This sentiment is a testament to our mission to heal, to discover and to educate.

Taleena, Caregiver
Challenge: Oxygen
A portable oxygen concentrator (POC) is a staple for lung disease patients around the world. However, their capabilities are misleading. Most POCs only deliver pulsed tone flow. This means the patient is delivered a bolus of oxygen each time they take a breath. While this may be sufficient for lung disease patients on low liter flows of oxygen, it’s not typically sufficient for patients needing 4 LPM (liters per minute) or more. Those patients usually need continuous flow oxygen to saturate properly. There are only a handful of POCs that deliver continuous flow oxygen and those machines cap out at two to three LPM. These POCs are marketed as a way to give patients their freedom back, however they are only sufficient for a subset of patients. They are even misunderstood by many in medicine, and thus prescribed to patients whose oxygen needs exceed what POCs can deliver. Because most POCs are pulsed tone only, those settings on the machine are not LPM, they are simply “numbers”. This again is another problem, as both doctors and patients think a POC set on 5 is delivering 5 LPM of oxygen. This is not the case. While impossible to determine an equivalent LPM between pulsed tone and continuous flow, the “written equivalent” for most POCs is just over 1 LPM. We need change. First, POCs need to be marketed and labeled properly. Second, we need POCs that deliver continuous flow oxygen at flow rates where PF patients can benefit.
Thore, Patient
Challenge: Oxygen
I was diagnosed at age 47 after a bout with pneumonia, and after a relapse in 2015, I now am oxygen dependent. The major obstacle is now being mobile with lousy options — bulky oxygen bottles or inadequate portable oxygen generators. After a while, there is a lack of real hope as you have to bypass trips, social functions and more because you always feel like you’re on a pitch count every time you leave the house. I have lived 23 years with it and the last five on oxygen have been the hardest.

Zaid, Family Member
Challenge: Treatment Options & Quality of Life
My name is Zaid and I am sharing my brief perspective as a family member, caregiver and in part, my mom’s primary healthcare provider and pharmacist. I lost my mom just last September. I was still just a student when she was diagnosed in late 2016 with idiopathic pulmonary fibrosis after her health had been deteriorating for some time. Due to my family’s financial constraints — and the unfortunately limited health services the public health sector in my country could provide — my mom wasn’t able to receive the earliest possible assistance nor the broader options for treatment that I wish she could have had. Almost any of the issues PF patients face can be considered as “most pressing”, but having witnessed the devastating effects of end-stage IPF (my mom’s words “If this cough can just leave” and “Help me! I can’t breathe!” still ring in my mind with a vivid image of her barely able to go to the bathroom and back without extreme dyspnea, despite the use of supplemental oxygen). This inclines me to believe that improved treatment options to alleviate persistent cough and treatments to improve lung function will drastically improve the poor quality of life outcomes that PF patients face.